UC Health has its sights set on improving the health of Californians by addressing everyday barriers to care.
For people with diabetes, this means considering the person’s whole situation and integrating the various aspects of care. This approach makes it easier and more rewarding for health care professionals and their patients.
Creating an integrated approach to diabetes management
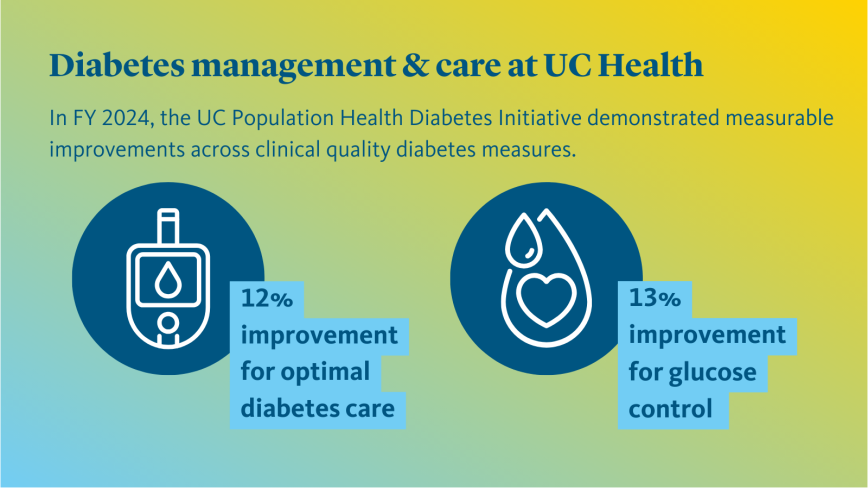
UC Health’s Diabetes Care Management Initiative, a systemwide program led by UC Population Health in collaboration with all six UC academic health centers, fosters real-time collaboration where UC site experts come together to identify and recommend improvements.
In partnership with the University of California’s Center for Data-driven Insights and Innovation (CDI2), the Diabetes Care Management Initiative has developed robust data dashboards that allow UC locations to compare and measure the impact of their work. This benchmarking enables UC care teams to identify, recommend and put in place approaches to care that are more likely to be followed by people with diabetes and, as a result, improve measures that track their condition.
Tailoring the approach to care
An important part of the Diabetes Care Management Initiative has been adapting care plans for the cultures and practices of groups of people who have diabetes but are not experiencing the same outcomes as others from the conventional system of diabetes care.
This plan involves increasing the use of educational materials that make sense in the cultures of the patients seen by the care teams. For example, education materials, such as videos, are made available in preferred languages, and patient language preferences are integrated into clinical workflows. Clinicians use targeted digital reminders for care and follow-ups.
One-stop integrated visits
Teams are working to make the management of this chronic disease easier for patients. The initiative helps to integrate testing protocols into the primary care visit that are critically important for diabetes management: blood glucose testing and eye examinations. By including these screenings in routine primary care clinic visits, patients no longer need to make separate trips to different facilities for these tests.
According to Christine Thorne, M.D., from UC San Diego Health and one of the leads of the Diabetes Care Management Initiative, “Combining as many of the routine tests that diabetic patients need into one primary care visit is crucial to helping them manage their diabetes. Reducing or eliminating the need for separate visits to different providers helps us work together as a team and maintain a more holistic view of their ongoing care plan.”
Other leads for the Diabetes Care Management Initiative include Matthew Freeby, M.D., and Maria Han, M.D., both from UCLA Health; and Katie Medders, Pharm.D., Ph.D., from UC San Diego Health, who is the UC Health pharmacist lead for the UC Population Health Pharmacy Group.
Another aspect of this integrated approach comes to life through UC Davis Health’s program in teleophthalmology, which helps integrate eye screening into routine care visits, especially with newly diagnosed diabetes patients.
Glenn C. Yiu, M.D., Ph.D., of UC Davis Health, and a pioneer in this field of study, notes, “Teleophthalmology provides a convenient way to get your eyes screened for diabetic retinopathy and other ocular disorders during a routine visit to the primary care physician.”
Diabetic patients receive their retinal screening exam as part of their regular primary care visit.
A remote location receives the tests and reads the results, returning them to the patient’s primary care provider in a timely manner. Co-location of retinal screening within the primary care setting removes a barrier to an integrated approach to delivering the care plan needed care for people with diabetes. Launched in 2018, this aspect of diabetes management is also available to patients at UC San Diego Health, UCSF Health and UCLA Health clinics.
UC Davis Health is also piloting a systemwide program integrating artificial intelligence to automate diabetic retinopathy grading. “Using AI provides real-time feedback,” says Dr. Yiu, “allowing patients to obtain necessary eye care in a more timely manner.”
A complex and far-reaching disease
Diabetes remains a leading chronic illness in the United States and ranks as the eighth leading primary cause of death among US adults in the country according to both the American Diabetes Association and the Centers for Disease Control. Some 38.4 million people in the United States, representing 11.6 percent of the national population, have the chronic disease, while approximately 3.6 million adults living in California (roughly 11.7 percent of the state’s population), have diabetes.
The disease’s impact reaches far beyond an individual’s blood sugar level. Long-term complications of diabetes often include cardiovascular disease, kidney disease, diabetic retinopathy, neuropathy and a host of other chronic conditions.
“While diabetes may not always be preventable, with early detection, intervention and treatment the disease can be managed and help to mitigate and sometimes eliminate its adverse effects,” according to Matthew Freeby, M.D., from UCLA Health.
That’s the approach that teams at UC Health locations have adopted and implemented to make it easier for people with diabetes to get the integrated care they need, as well as to assist in early detection and disease management.
Advancing a team-based, integrated approach to diabetes management
The Diabetes Care Management Initiative has also shown how providing care through a team-based model can lead to better care.
Another critical focus area for the care of people with diabetes centers on a team-based care model where pharmacists are embedded in a person’s interdisciplinary diabetes care team. This model refocuses the role of the pharmacist from being solely responsible for dispensing medication to one that can provide critical patient education, care responsibility counsel and chronic disease management support.
This team-based approach with a pharmacist in the mix can result in better outcomes, fewer side effects and an overall lower cost of care. A study and research specific to diabetes management also points to the positive impact that including a pharmacist in a diabetes patient care team can have, such as increased medication treatment adherence, better outcomes, tailored education and improved disease state management.
“Involving a pharmacist in a patient’s care plan supports a clinical care pathway to help get patients on the right medications. It supports a comprehensive view of the patient and points toward a more proactive, preventive care model,” shares Katie Medders, Pharm.D., Ph.D., from UC San Diego Health.
An additional study led by Kimberly Narain, M.D., Ph.D., MPH, from UCLA Health found that patients who got personally-tailored help from pharmacists to take their medication correctly along with care from their primary care physician (a program called UCMyRx) had better control of their diabetes after one year, compared to patients who received care only from their primary care physician. These customized strategies helped people stay on track with their medications by addressing problems such as costs, trouble getting to appointments and confusion about how to take prescriptions.
In particular, the study found that “having at least one UCMyRx clinical pharmacist visit was associated with a decline in blood sugar similar to what would be expected for adding on a new diabetes medication.”
The pharmacist integration and other aspects of the Diabetes Care Management Initiative are part of an important focus on an integrated, whole-person model to remove barriers and increase access for overall positive patient outcomes.
Both the American Diabetes Association and the American Heart Association support these approaches that UC Health has been advancing.
In its “Standards of Medical Care in Diabetes” position statement, the ADA recommends a patient-centered, team-based approach to caring for patients with diabetes. The American Association of Nurse Practitioners takes a similar view, stating “Whether a primary care provider is a physician, NP or PA [physician assistant], a treatment plan’s success is dependent upon a collaborative team and an informed, activated patient. Initiatives such as the Patient-Centered Medical Home help support comprehensive primary care and offer new opportunities for team-based diabetes management.”
Looking forward
The Diabetes Care Management Initiative is just one of several initiatives of the UC Population Health program designed to help improve the everyday health of people in California.
From hypertension management to coordinated care, these initiatives strive to provide quality access to care with as few barriers as possible to the broadest number of people in the state.
About University of California Health
University of California Health comprises six academic health centers, 21 health professional schools, a Global Health Institute and systemwide services that improve the health of patients and the University’s students, faculty and employees. All of UC’s hospitals are ranked among the best in California and its medical schools and health professional schools are nationally ranked in their respective areas.