A first-generation university student and the son of Mexican immigrants, Assistant Professor Fabian Rivera-Chávez was born and raised in Northern California. He joined UC San Diego’s faculty in the School of Medicine and the Division of Biological Sciences in October 2020, in the midst of a global pandemic as the world struggled to work its way out of COVID-19 devastation. He recently worked alongside colleague Dr. Alli Weis at the University of Utah School of Medicine to publish an article in Spanish in the Los Angeles Times about vaccine safety, part of his efforts to communicate the importance of vaccination in underserved communities.
Q: What is the focus of your research?
A: My research is focused on understanding how intestinal bacterial pathogens, such as Vibrio cholerae and Salmonella, promote their own growth in the gastrointestinal tract during infection, and how this enables them to transmit to a new host. Our research may shed light into the development of novel and cost-effective therapeutics for treating and preventing infectious diseases.
Q: What was your motivation in working with Alli Weis in producing a story in Spanish about vaccine safety?
A: There is a lot of misinformation surrounding COVID-19 vaccines. There is also a lack of outreach to Spanish-speaking Hispanic communities in the U.S regarding COVID-19 and the vaccines. COVID-19 disproportionately impacts Black and Latino populations: they are about three times as likely to contract the virus and about twice as likely to die from COVID-19 compared to non-Hispanic whites. However, while communities of color in the United States are at higher risk for fatal COVID-19 infections, recent studies have shown that non-Hispanic whites are being vaccinated at twice the rate of Blacks and almost three times the rate of Hispanics in the U.S. I have personally lost family members and family friends to COVID-19. Therefore, I believe that it is my duty as a Mexican-American scientist to involve myself in the outreach to these communities.
Q: Why is it critical to help communicate the importance of vaccination in underserved communities?

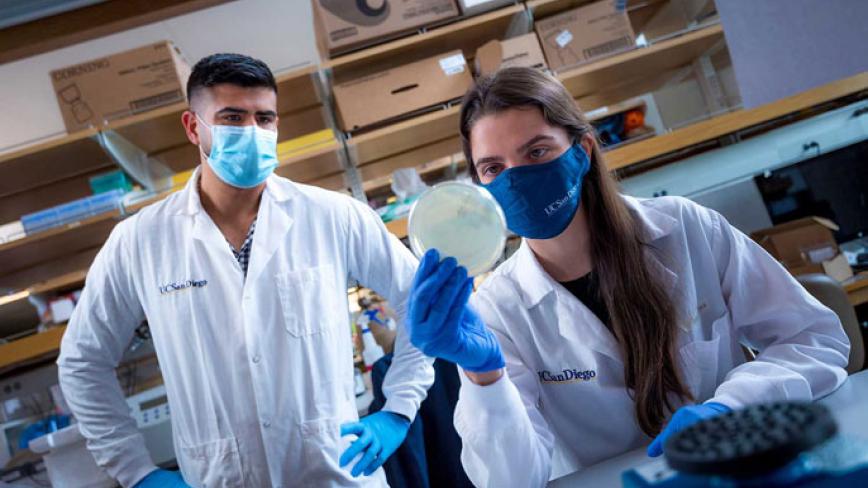
Credit: Erik Jepsen/University Communications
A: Since people of color in underserved communities are disproportionately at risk for contracting and dying of COVID-19, it’s extremely important to educate these communities on the importance and safety of COVID-19 vaccines. The lack of outreach combined with misinformation has exacerbated vaccine hesitancy in historically marginalized communities of color. If we want to achieve vaccine equity and reduce mortality in these populations, we need to do more direct outreach to these communities. UC San Diego Health has made progress in this regard in collaboration with community-based organizations with the “Mobile Vaccine Clinic,” which aims to expand outreach and enhance the distribution of COVID-19 vaccines to San Diego County communities of color that have been disproportionally impacted by the pandemic.
Q: Why is there more apprehension in Spanish-speaking and other underserved communities in trusting vaccine safety?
A: There is a long history of medical abuse and maltreatment of Black and Hispanic communities in the United States. This is at the root of vaccine hesitancy. Therefore, we need to first acknowledge this and work hard to earn back the trust of these communities. Hispanic communities are also fearful of interacting with the government because of recent anti-immigration policies and sentiments. Thus, it’s important for us to approach the issue of vaccine hesitancy with empathy and understanding, not with coercion and judgement. There is also a lot of misinformation surrounding COVID-19 vaccines on social media, which further fuels vaccine hesitancy.
Q: What’s most important to communicate to those who feel the COVID-19 vaccines were rushed to approval or not 100 percent effective?
A: First of all, no vaccine is 100 percent effective, but the COVID-19 vaccines licensed in the U.S are very safe and the mRNA vaccines are approximately 95 percent effective at protecting you from infection, which is about as good as a vaccine can get. Importantly, these vaccines are very effective (up to 100 percent) at protecting you from severe disease. Although the COVID-19 vaccines may seem rushed, they are not. The vaccines are the product of decades research and have undergone rigorous safety and efficacy testing (phase 1-3 clinical trials). The bar is very high when it comes to approving vaccines in the U.S and the COVID-19 vaccines have not skipped any safety or efficacy tests that would normally be required. In order to be approved by the FDA, vaccines have to be virtually 100 percent safe and provide at least 50 percent protection. Although we won’t have an answer about long-term safety of the vaccines for some time, there is no scientific or medical reason to worry about any long-term side effects of the vaccines. These vaccines are not based on live virus, and they protect you by training your body to make antibodies against a single viral protein. One thing is for certain: there is a clear benefit to getting vaccinated and it’s much less risky to your health than getting the actual infection.
Q: How long do the current COVID-19 vaccines last?
A: This is an important question and time will tell but the most recent data indicate that the neutralizing antibodies elicited by the Moderna and Pfizer mRNA vaccines last for at least six months, which is excellent news. These studies are ongoing and will continue to look at the protection over time, so we don’t yet know exactly how long vaccine protection lasts. It could be much longer than six months but we will have to wait to find out.
Q: If I had COVID-19 in the past, do I need to get vaccinated?
A: The answer is, yes, you still should. The main reason is because the immunity to natural SARS-CoV2 infection varies depending on how much virus you were exposed to. Some people may have no antibodies after infection, while others can have high levels of antibodies. This is especially important with respect to variants, because the high and consistent level of antibodies after vaccination may lead to better protection. Also, there is no harm from getting vaccinated if you have been infected, so it can only help.
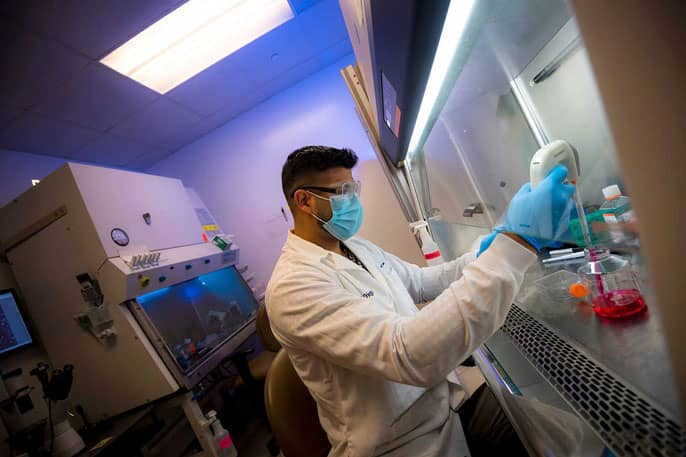
Credit: Erik Jepsen/University Communications
Q: Will the COVID-19 vaccines provide protection against the emerging variant forms of the virus?
A: So far, the vaccines licensed in the U.S have been found to be effective against all the known major variants (or strains) that have emerged so far. Importantly, all three vaccines licensed in the U.S. (Pfizer, Moderna and Johnson & Johnson) have been shown to be effective against B.1.1.7, which is currently the dominant strain in the U.S. However, it’s impossible predict what new strains or variants will emerge and whether new strains will have the potential to evade vaccine immune responses. The good news is that mRNA vaccine technology allows for these vaccines to be reformulated within weeks of determining a new variant's sequence, which would theoretically allow for the rapid production of a new, protective vaccine. If you are getting the Pfizer or Moderna vaccine, it’s important not to skip the second dose because this “booster” dose elicits 10 times more antibodies than the first dose. These higher levels of antibodies may provide greater protection against emerging variants. Time will tell how effective these vaccines will be in the long-term against any new variants but so far, the data look very promising. Vaccines are the best tool we have to defeat the pandemic. As we continue to vaccinate more people, we will continue to get closer and closer to a semblance to normalcy.
Rivera-Chávez earned a bachelor’s degree in molecular, cell and developmental biology from UC Santa Cruz. He earned his Ph.D. in microbiology from UC Davis. He completed postdoctoral research at Harvard Medical School before joining UC San Diego’s faculty in 2020.