On New Year’s Eve 2019, as the rest of the world popped champagne corks and prepared to usher in a new decade, Dr. Carrie Byington was looking ahead at something much more disturbing on the horizon.
She was just a few weeks into her new role overseeing UC’s vast health system, when news began to emerge of a new virus infecting people halfway around the globe. As an infectious disease specialist with international expertise, she realized right away that the threat could soon be headed to California.
Over the next few weeks, she and other UC leaders marshalled expertise and resources from across the university to help both UC and public health authorities respond. In short order, UC helped identify some of the first COVID-19 cases in the U.S. from community spread, prepared UC’s statewide network of hospitals to meet an expected surge in patients and helped meet an urgent demand for diagnosis and testing.
“I told my team that whatever the state asks of us, our answer will be yes,” Byington said.
Reflecting on the one-year anniversary since California enacted a hard shut down to curb the pandemic, Byington spoke about UC’s efforts to address the health crisis, where we go from here, and lessons learned from this extraordinary year.
Q: When was the moment you first realized the seriousness of this new virus?
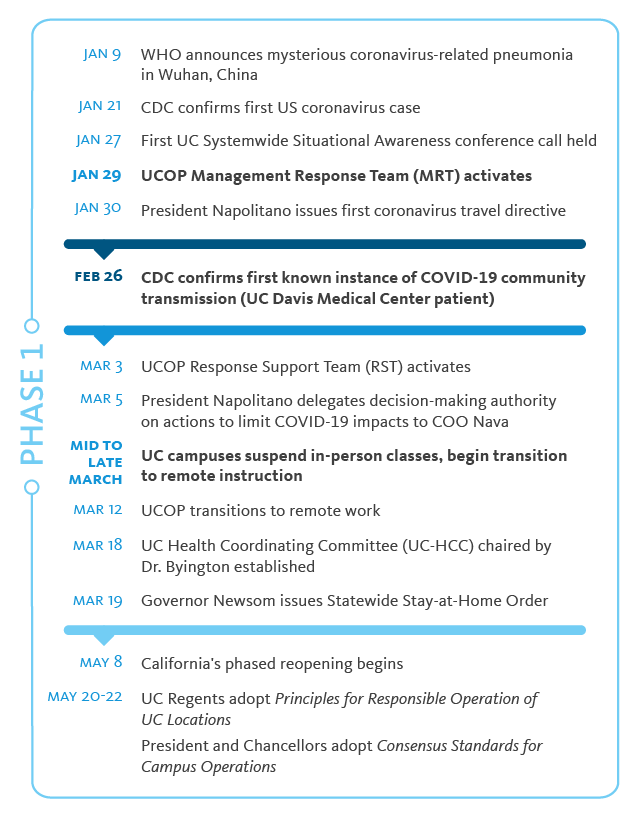
A: Dec. 31 is the first day I heard about cases of a novel virus and pneumonia emerging in Wuhan, China. On January 1, I called [then] UC President Janet Napolitano and said, “What does UC have systemwide to address an emergency?”
I was really trying to understand what resources were available to address what I knew would be a problem that could affect our entire system, and our entire state.

Credit: University of California
I called on UC’s Management Response Team, a systemwide group which guides policy decisions during a crisis. We were able to use the infrastructure and experience the team had developed during emergencies such as wildfires and earthquakes to help us respond to the growing health crisis.
As an infectious diseases physician, I knew one of the very first things we had to do was figure out how we could diagnose the infection and treat the disease. I found out there was a systemwide group of pathologists that we could work with and say, ‘OK, we know there is a new virus, how are we going to test for it?’
The other groups I started to bring together right away were infection prevention and public health, because we knew we needed to think about how to protect our hospitals, our patients, our health care workers and our campuses.
I can remember meeting with our health center CEOs and asking, ‘What would you do if 10 or 20 percent or even more of your patients had COVID?’ I was a new leader and at the beginning, they might have thought I was out of my mind! But I knew, this was what we had to prepare for. A pandemic was coming.
Q: How did having a coordinated response across UC help the state respond to the unfolding crisis?
A: The decisions you have to make during a pandemic — these are decisions that affect everyone, and consistency is key to getting your message out, to keeping people safe and to ensuring we’re working in a similar way at each location.
On March 18, we started the UCH Coordinating Committee (UCH-CC) to guide UC’s systemwide response. But this group had really been working since the first week of January. Leveraging the power of our 10 campuses meant we had some of the best expertise in the United States together, in the same room (or on the same Zoom).
Q: Early on, most cases involved people who had traveled abroad. But by February 2020, limited testing capabilities meant it was difficult to know whether it was spreading domestically. How did UC respond?
A: We had been meeting with infectious disease experts inside and outside of UC, and by then, we all knew that there must be community spread. But we just weren’t able to diagnose it because we didn’t have the diagnostic tools.
We talked among ourselves about what were some of the best ways we could recognize if we had a patient come in with COVID-19.
We agreed that if a patient came in very sick and tested negative for influenza and other common viruses on traditional respiratory panels, we should be suspicious that they might have the novel coronavirus.
It turned out that UC Davis on February 26, 2020, identified the nation’s first patient with COVID-19 acquired from community spread. They were able to use their expertise and strongly advocate to the CDC that this patient needed to be tested, even though there was no history of travel.
Q: Once it was clear that COVID-19 was spreading in our communities, the need for reliable diagnostic testing really accelerated. What was UC’s role?
A:Early on, we knew that we could develop a polymerase chain reaction (PCR) test to identify the novel coronavirus. We were able to compare notes and share information and even samples of RNA. We advocated with the CDC and FDA to allow clinical laboratories to develop tests and to use these tests for our patients. Our health centers worked together and began to validate tests of the coronavirus at each of the locations.
The FDA issued guidance for clinical labs on February 29, 2020, and within 12 days, all of our clinical laboratories began offering testing under emergency use authorization.
Today, we’ve tested more than one million people. About half have been our patients at our health centers. The rest of the tests were done for California public health laboratories, for special populations like the homeless, those in nursing homes, first responders, agriculture workers, and UC students and employees.
Q: UC has also played a leading role in clinical trials for potential treatments and vaccines. Can you tell us more about that?
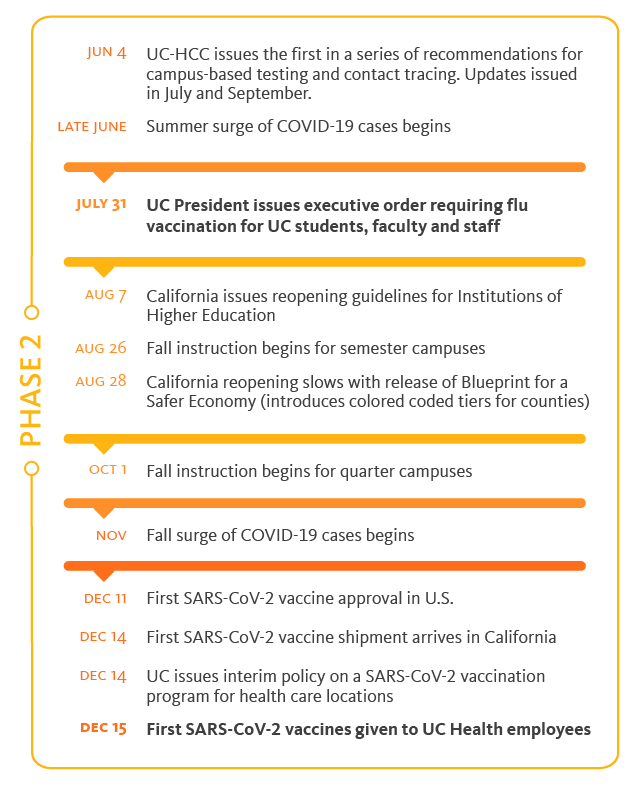
A: The impact has been huge. From the beginning, the UC Health Coordinating Committee worked to coordinate clinical trials across the system. We wanted to participate in all vaccine trials and high-impact drug trials because of the imperative to find the treatments and the vaccines to end this pandemic. If we entered trials in a piecemeal way, then everyone would be competing for the same patients. By coordinating and choosing high impact trials, we were able to enroll the largest number of people, which helped the trials moved forward more quickly.
In our trials, we focused on enrolling diverse populations using the trusted relationships that many of our UC investigators had developed across California communities. Our participation helped our patients get access and also allowed us to contribute critical data to national trials.
Q: How is UC able to reach underserved communities?
A: We have a very strong health professional faculty and teams of staff, trainees, and students at every location that have worked with community partners, sometimes for decades. We had built up trust in many communities in California before the pandemic and that’s a unique asset.
The other asset that UC brings is the exceptional investigators we employ. These investigators were able to generate and analyze data that could then be used to inform decisions and policy-making to improve the lives of patients in diverse communities.
Q: What role did UC Health play in helping keep students and employees on our campuses safe?
A: As we were thinking about return to campus, we had three systemwide goals: One, that each campus was at least as safe and preferably safer than the surrounding community; two, the campuses would not be a source of transmission into the surrounding community; and three, that we would have no deaths among students or employees when students returned in Fall of 2020.
One of the things I tried to do with the UCH-CC was to bring systemwide expertise together to coordinate decisions on the big principles, without inhibiting innovation on individual campuses.
We gave guidance to the campuses that they had to reduce population density on campus to a level where they could support testing of anyone with symptoms, periodic asymptomatic testing, contact tracing, and supported isolation and quarantine for their students and employees. We recommended non-pharmaceutical interventions on each campus including mandatory masking. We also recommended each campus develop a pledge to healthy behavior and ask their communities to adopt it.
All of these standards and recommendations helped us to meet our goals to keep our students, employees and communities safe.
Q: What comes next in terms of helping California move beyond the pandemic?
A: At this point in the pandemic, we have learned many lessons. There are lessons for us as a system including how to collaborate and use data for making decisions, as well as a renewed commitment to health equity and improving the health of all Californians.
Going forward, I see the UC system playing a bigger role as a partner for the state. We can use our data, our expertise and innovations to reach more people, improve access and deliver on the promise of good health.
Q: Are we better prepared now for another health crisis?
A: When the pandemic is finally declared to be over, we will move forward as a stronger and more prepared institution.
Our system-level decision-making has been strengthened. We now have an enterprise data warehouse for health across the system that is updated daily. It lets us know: How many patients we have with COVID, how many beds including ICU beds are available across the whole system, how many ventilators, vaccines and even pieces of PPE are available and where are they located.
We rely on these data to manage the day-to-day operations of the pandemic and can now use these resources to better manage other diseases and the health of populations.
Our use of technology is different today and we are certainly using it to improve patient access, equity and experience as a result of COVID.
Following the pandemic, preparedness and health security will take on an entirely new level of importance. We are not going to lose these lessons.
UCH in the fight against COVID-19
Hear the story of UCH's work to help end the pandemic. Dr. Carrie L. Byington discusses UCH milestones and accomplishments.